
A colonoscopy is a screening procedure used to offset the risk of colorectal cancer. While some healthcare systems recommend its use as a preventative diagnostic tool, others recommend less invasive alternatives.
For instance, the American Society for Gastrointestinal Endoscopy (ASGE) recommends a colonoscopy every 10 years starting at age 45 or 50 depending on risk factors like age and family history. But some people may be reluctant to opt for this diagnostic procedure due to fear of common complications.
Whereas, the Canadian Taskforce on Preventative Health Care recommends gFOBt and FIT (both are stool tests) every two years or a flexible sigmoidoscopy every 10 years (less invasive than a colonoscopy).
Post-colonoscopy digestive issues like constipation, diarrhea, bloating, etc., may develop, that are similar to symptoms following gut cleansing methods like colon irrigation and colon cleanses using teas and laxatives. Let's look into a few of the less talked about aftereffects of colonoscopy, underlining the surprising efficacy of probiotics in mitigating long-term complications and bolstering overall gut health.
What is a colonoscopy? What is a colonoscopy used for?
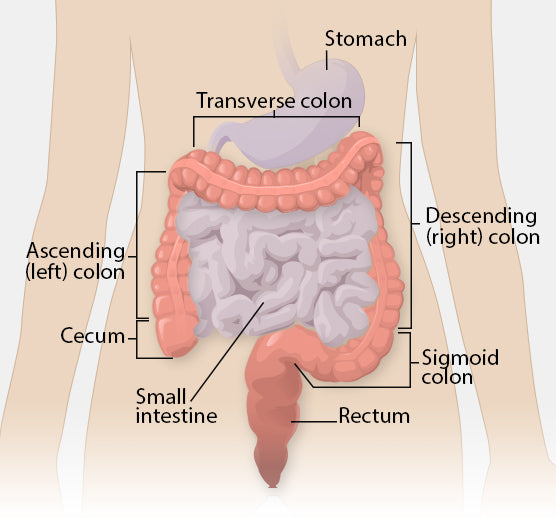
A colonoscopy is an investigative medical procedure that uses a colonoscope (a camera at the tip of a long, flexible tube) to see the insides of your large intestine (colon, rectum, and anus) for any abnormalities.
A colonoscopy may be used to diagnose gastrointestinal issues such as intestinal bleeding, colon polyps (harmless cell growths that may be early signs of cancer), inflammation, and inflammatory bowel disease, or to take a tissue sample (biopsy) from the large intestine for colorectal cancer screening.
Bowel preparation before a colonoscopy
Good bowel preparation includes prepping your colon several days in advance by following a special diet that will avoid high-fiber foods and following up with a clear liquid diet the day before the colonoscopy. To see your bowels clearly and catch any abnormalities, the night before the colonoscopy, you will be recommended to take a laxative like PEG or saline-based laxatives that will help to clear out your bowel completely and increase visibility.
Osmotic laxatives like PEG are large molecules that cannot be absorbed by your gut, which encourages your gut to draw in water and electrolytes and expel softened stool as quickly as possible. While laxatives help clear out the gut, they can also lead to electrolyte imbalances and dehydration. Most laxative kits come with an electrolyte component, either as a recommendation to take the laxative with a sports drink or as a combination of osmotic laxatives and electrolytes.
Additionally, not all laxatives are equally effective. Based on your medical history, you may be recommended a specific type of laxative. For instance, combination laxative (PEG with ascorbic acid) are avoided for those with a glucose-6-phosphate dehydrogenase deficiency.
PEG — Can it cause an allergic reaction?
Polyethylene glycol (PEG) is a synthetic polymer widely used as an additive in pharmaceutical, cosmetic, and food industry. PEG is also used as a laxative for bowel preparation before colonoscopy and bowel surgery. Although allergic reactions to PEG are quite rare, recent investigations suggest that PEG may lead to mild hypersensitive reactions like urticaria (hives, itching, and swelling), to life-threatening anaphylactic shock (difficulty breathing, swelling of the throat and tongue, a drop in blood pressure, rapid pulse, skin hives or rash, and dizziness).

PEG is the preferred recommendation for those who have preexisting electrolyte imbalances (history of renal failure, heart failure or cirrhosis) and those with IBD and cannot tolerate saline-based laxatives.
Can saline-based laxatives lead to electrolyte imbalances?
Saline based laxatives include salts like magnesium citrate, sodium sulfate, and sodium phosphate. Sodium phosphate and magnesium citrate have been associated with severe electrolyte balance-associated side effects like hyperphosphatemia and magnesium toxicity in those patients who have a history of electrolyte imbalances.
Combination laxatives used for bowel prep like sodium picosulfate/magnesium citrate and low volume PEG with ascorbic acid have been associated with increased rates of abdominal pain, nausea, and vomiting and vomiting, respectively.
What are some post-colonoscopy complications?
A colonoscopy may assist in detecting gastrointestinal conditions like inflammation, IBD (Crohn's and Ulcerative Colitis), causes behind rectal bleeding, or as a tool for early colon cancer screening and large polyp removal.
Most colonoscopies occur without significant side effects. But, data from a University of Washington, Seattle study and a review discussing global trends in adverse events related to colonoscopy published in World Journal of Gastroenterology suggest:
- Colon perforations are linked with high mortality rates, with perforation rates ranging from 0.005% to 0.085% (covering more than 50,000 colonoscopies)
- Post-colonoscopy bleeding occurs in roughly 0.001 to 0.7 cases.
- There are approximately 5-7 serious adverse events per 1,000 colonoscopies, and post-colonoscopy complications increase in elderly patients and those with IBD.

Serious adverse events include abdominal pain, bowel perforation, hemorrhage, death, and other less specific hospitalizations. Some colonoscopy complications may include:
Bleeding and perforations
To perform the colonoscopy, your doctor may inflate the bowels either with water or some type of gas (CO2). If the bowels are overextended due to this inflation, a mechanical injury due to the scope itself, or if the wound hasn't sealed properly after polyp removal, a perforation (tear in the intestinal wall) may occur.
Although rare, an intestinal perforation can lead to severe complications like continued bleeding, inflammation (peritonitis), and sepsis. Perforations occur in roughly 0.08% for every 50,000 colonoscopies and bleeding, a more common symptom associated with polyp removal, can occur in roughly 35 patients for every 50,000 colonoscopies.
Moreover, according to a multivariable analysis, the risk for bowel perforation increases with age, anesthesia class, female sex, polyp size, and whether the procedure was performed by a gastroenterologist or an endoscopist of an unknown specialty.
Bad reaction to anesthesia
The risk of complications increases when sedative drugs are used. Compromised cognitive recovery including short-term postoperative cognitive dysfunction (delirium includes inattention and confusion) and long-term postoperative neurocognitive disorders (including delirium, mild to severe reduction in mental function or dementia) are a recognized concern after surgery and anesthesia in elderly patients.

Generally, you may be provided with a choice in degree of sedation and/or anesthesia. While most people opt for anesthesia, you also have the option for light and moderate sedation. If you have ever had a bad reaction to anesthesia, you should inform your doctor, as severe reactions to anesthesia may result in stroke, heart attack, respiratory distress, and death.
Post-colonoscopy abdominal pain, bloating, pelvic cramps, and post-polypectomy electrocoagulation syndrome (PPES)
To remove any polyps, your endoscopist uses surgical tools (colonoscope and ESU/Electrosurgery generator unit) to see and destroy polyps and to seal the wound to prevent bleeding. This process may sometimes lead to a deeper burn that results in pain, infection, inflammation, and cramps post-colonoscopy. This is called post-polypectomy electrocoagulation syndrome and is one of the most common complications of a colonoscopy.
Or, your doctor may use a suction device to remove the polyp. This may lead to some tugging on the intestinal wall and may lead to you feeling some discomfort and belly pain for a few days after your colonoscopy. If you notice blood in your stool, persistent abdominal pain, and cramping, or if you develop a fever and chills, inform your physician immediately.
Typically, these symptoms resolve within a few days with adequate bowel rest (including an easily digestible diet including soft foods like mashed potatoes, applesauce, etc., and avoiding greasy foods and high fiber foods) and antibiotics like cephalosporin, amoxicillin, ciprofloxacin and/or metronidazole.
Antibiotics like fluoroquinolones may have severe side effects (commonly called being floxed) like tendinopathy and tendon rupture. Tendons are connective tissue that connect muscle with bones. Additionally, antibiotics exposure (especially quinolone antibiotics) around the time of colonoscopy (this study suggests within 2 weeks of a colonoscopy) may have a slightly higher risk of developing irritable bowel syndrome (IBS).

Electrolyte imbalance
Laxatives, used in the bowel prep phase, draw in water and electrolytes from the rest of the body to ease their passage through the bowels. This and the restricted diet before and after (polyp removal) may exacerbate an electrolyte imbalance, if not sufficiently addressed.
Mild symptoms of an electrolyte imbalance post colonoscopy may look like headache, nausea, and constipation, while more severe symptoms can include seizures, paralysis, and coma.
Generally, bowel prep kits will either recommend you take the laxative with a sports drink or come with electrolyte supplements. You can also make an electrolyte rich sugar-free/low-sugar electrolyte drink at home with simple ingredients like cream of tartar, pink Himalayan salt and lemon juice, and coconut water.
Bacterial infections
A recent study reported that bacterial infections post colonoscopy and upper gastrointestinal endoscopy performed in an outpatient setting like ambulatory surgery centers (ASCs) are more common than previously thought. Roughly 1 and 1.6 infections for every 1000 procedures were reported for screening and non-screening (diagnostic colonoscopy) procedures that were reported seven or fewer days after a repeat colonoscopy procedure.
The most common infections (E. coli, Klebsiella, and Enterobacteriaceae) following endoscopy (upper GI and colonoscopy) may occur either due to a contaminated colonoscope or via bacterial translocation - case studies suggest damage to the intestinal mucosa may allow intestinal bacteria to move into deeper tissue (lamina propria) or enter the blood supply leading to infection.

Symptoms of bacterial infection after colonoscopy
Some bacterial infections may be asymptomatic (show no outward signs) while others may overlap with post-colonoscopy abdominal discomfort. Some signs of bacterial infection may include:
- Bloating and gas
- Belly pain
- Fever and chills
- Irregular bowel movements
- Diarrhea
- Nausea
- Vomiting
In some rare cases, gas, bloating and bowel irregularity can continue for an extended period. Often, doctors will recommend repeated courses of antibiotics in attempts to address the issue. However, each additional course of antibiotics can make it difficult for your microbiome to recover.
Dr. Martin Blaser’s research suggests that there are certain classes of antibiotics called macrolides can disrupt microbiome recovery even after a single dose. A reduction in gut microbiome diversity due to bowel prep and antibiotic therapy may allow pathogenic bacteria like C. difficile to gain a foothold in the gut. Research suggests consumption of probiotics along with antibiotics may help reduce the risk of AAD (Antibiotic associated diarrhea) or C. difficile infections (CDI).
Role of probiotics in recovering from colonoscopy and in long-term colon health
Bowel preparation or colon cleansing is essential for a successful colonoscopy, but it can also impact your gut microbiome composition and the synthesis of vital metabolites like short chain fatty acids (SCFAs). Additionally, there may be an increased risk of antibiotic-associated diarrhea (ADD), if you’ve been prescribed antibiotics.
A study looking at the difference in gut microbiome diversity before and after a colonoscopy found that there’s a significant reduction in gut microbiota composition immediately after a colonoscopy that can take up to 2 weeks to stabilize completely.

Although some research did not find a significant change in gut microbiota diversity, other studies suggest that there may be long-lasting effects on Lactobacillaceae abundance, as well as a significant increase in gram-negative Proteobacteria immediately after the procedure.
Overgrowth of Proteobacteria - Is it bad?
Gram negative bacteria are not inherently bad bacteria, but when there’s an imbalance in the gut microbiome that allows certain groups of gram negative bacteria like Proteobacteria to increase without competition, it has been associated with several ill health effects including metabolic disorders and inflammatory bowel disease.
For instance, certain Proteobacteria species such as E. coli shed an endotoxin known as lipopolysaccharides (LPS). A healthy gut wall has an inbuilt mechanism that helps inactivate LPS, but a compromised gut wall may allow still active LPS to pass into the blood stream. LPS is a potent proinflammatory trigger and has been associated with increased oxidative stress, low-grade endotoxemia, inflammation, cardiovascular events (damage to the heart muscle) in patients at risk and metabolic syndrome.
Taking probiotics before and after a colonoscopy had a positive impact on gut microbiome recovery with a reduced number of days with constipation, pain, bloating, diarrhea, and general discomfort.
A double-blind clinical trial found that a multi-strain probiotic might facilitate faster recovery from adverse events like belly pain, cramps, heartburn, diarrhea, nausea, vomiting, bloating, and constipation after colonoscopy.

The species in the trial B. bifidum, B. lactis, E. faecium, L.acidophilus, L. rhamnosus, and L. lactis were selected for selective beneficial properties like resistance to stomach acid and digestive enzymes, pathogen inhibition, inhibition of C. difficile, improved barrier function and facilitating a regulatory effect on immune cells.
Rich in targeted strains, our probiotics Ideal Immunity® and Antibiotic Antidote® are both designed to work cohesively and help rebuild your gut. Learn more about the strains in Ideal Immunity® to help defend against pathogens and protect your immune system here, and the strains in Antibiotic Antidote® to target free radicals generated by antibiotic use and strengthen mucosal lining in the gut here.
Frequently Asked Questions
What happens if a colonoscopy goes wrong?
A colonoscopy may lead to a few post-colonoscopy complications like perforations, bleeding, bad reactions to anesthesia, bacterial infections, electrolyte imbalance, etc. Other common complications may include bloating, nausea, vomiting, cramps, heartburn, constipation, and diarrhea.
What is the most common complication of a colonoscopy?
The most common complications include abdominal discomfort including pain, bloating, constipation, cramps, diarrhea, nausea, etc.
How common is a failed colonoscopy?
4% to 25% of colonoscopy procedures may remain incomplete due to various reasons like limited visibility due to improper bowel prep, bowel issues such as diverticulitis, etc.
How do you know if you have an infection from a colonoscopy?
Abdominal pain that lasts longer than a week, fever, chills, diarrhea, etc., may signal an infection after a colonoscopy.
Can you become septic after a colonoscopy?
Yes, if you’ve had a polyp removed, or there’s been an accidental perforation, it may become infected and if left untreated, may lead to sepsis.
With gratitude,

 Martha Carlin, is a “Citizen Scientist”,
systems thinker, wife of Parkinson’s warrior, John Carlin, and founder of The BioCollective , a microbiome company expanding
the reach of science and BiotiQuest, the first of it’s kind probiotic line. Since John’s diagnosis in 2002,
Martha began learning the science of agriculture, nutrition, environment, infectious disease, Parkinson’s
pathology and much more. In 2014, when the first research was published showing a connection between the gut
bacteria and the two phenotypes of Parkinson’s, Martha quit her former career as a business turnaround expert
and founded The BioCollective to accelerate the discovery of the impact of gut health on all human disease. Martha was a speaker at the White House 2016 Microbiome Initiative launch, challenging the scientific
community to “think in a broader context”. Her systems thinking background and experience has led to collaborations
across the scientific spectrum from neuroscience to engineering to infectious disease. She is a respected out of the
box problem solver in the microbiome field and brings a unique perspective to helping others understand the
connections from the soil to the food to our guts and our brains.
Martha Carlin, is a “Citizen Scientist”,
systems thinker, wife of Parkinson’s warrior, John Carlin, and founder of The BioCollective , a microbiome company expanding
the reach of science and BiotiQuest, the first of it’s kind probiotic line. Since John’s diagnosis in 2002,
Martha began learning the science of agriculture, nutrition, environment, infectious disease, Parkinson’s
pathology and much more. In 2014, when the first research was published showing a connection between the gut
bacteria and the two phenotypes of Parkinson’s, Martha quit her former career as a business turnaround expert
and founded The BioCollective to accelerate the discovery of the impact of gut health on all human disease. Martha was a speaker at the White House 2016 Microbiome Initiative launch, challenging the scientific
community to “think in a broader context”. Her systems thinking background and experience has led to collaborations
across the scientific spectrum from neuroscience to engineering to infectious disease. She is a respected out of the
box problem solver in the microbiome field and brings a unique perspective to helping others understand the
connections from the soil to the food to our guts and our brains.


Waking Up to a Probiotic Breakfast Can Do Wonders for Your Gut Health
Did you know that recent studies show people with poor gut diversity had lower quality of life? The health of your microbiome impacts your mental health, sleep, energy, the risk for chronic illnesses, and much more. A probiotic breakfast can...

Can Probiotic Supplements Make or Break Your Fast?
Intermittent fasting (IF) may have started as a fitness trend for weight loss, but today it's a go-to lifestyle choice for many. Practicing intermittent fasting has been linked with health benefits such as lowering blood sugar and insulin, preventing heart...












 Martha Carlin
Martha Carlin






